New Study Reveals: Millions of Expectant Mothers in the US Face Limited or No Access to Prenatal Care
A staggering 5.6 million women of a reproductive age in the United States are currently grappling with poor access to prenatal care, a concern exacerbated by the increasing rate of what's termed "maternity care deserts". According to a comprehensive research report by March of Dimes, 36% of counties across the US now fall under the classification of "maternity care deserts" (which means, they don’t have any birthing centers or obstetric service providers). Moreover, this recession and high cost of living are not helping things.
This report from March of Dimes has been published in the midst of a US healthcare sector that is wrestling with a significant lack of access to maternal health. Multiple independent studies have underscored that the US suffers from the most unfavorable maternal health outcomes and the most pronounced maternal health disparities among developed nations.
Dr. Elizabeth Cherot, President and CEO of March of Dimes, emphasized that a person's ability to have a healthy pregnancy and birth shouldn't be determined by their geographical location and access to consistent, high-quality care. With that said, this report illustrates that today these very factors jeopardize the lives of countless women in the US during pregnancy and childbirth.
Cherot further stated that their research demonstrates that maternity care is not adequately prioritized within the healthcare system, and immediate measures must be taken to ensure that all mothers receive the necessary care they deserve to facilitate healthy pregnancies and robust baby health.
The study noted an increased risks to the babies born in these areas. Necessarily, this will mean there is an increased risk of birth injuries such as cerebral palsy and HIE if proper prenatal and obstetrical care is not provided to the expectant mothers.
A Worrying Trend of Closure of Labor and Delivery Units
A striking 5.6 million women in their reproductive years live in counties where maternity care services are either absent or notably limited. This trend is largely attributed to the closure of labor and delivery units in hospitals. Since the initial coverage of this topic by March of Dimes in 2018, as many as 369 counties have witnessed the shutdown of their obstetric units and labor and delivery suites, constituting roughly one in ten counties.
An additional 70 counties in the US have now been branded as maternity care deserts following the closure of obstetric wards since the 2018 report. Collectively, more than one in three US counties now fall within the category of maternity care deserts, characterized by the absence of hospitals or birthing centers providing obstetric care, and devoid of obstetric service providers.
The authors of the report attribute the closure of obstetric wards to factors such as escalating operational costs. The report cites statistics from the American Hospital Association to highlight that only about 50% of births in maternity care deserts are reimbursed through Medicaid, which offers lower compensation compared to private insurance.
This renders obstetric wards prime targets for closure in hospitals dealing with narrow profit margins.
Dangers to the Health of the Expectant Mother and the Baby
Regrettably, this national problem is severely detrimental to the health of the expectant mother. Researchers underline that over 32 million women in their reproductive years are susceptible to compromised health outcomes due to their inability to access reproductive healthcare services. This issue is most acute in rural states.
The presence of chronic illnesses substantially contributes to health outcomes, the study authors suggest. Eight out of ten maternity care deserts have a significant concentration of expectant mothers struggling with chronic ailments, some of which exert a direct impact on birthing conditions like preeclampsia (maternal high blood pressure) and premature birth. Many of these preventable conditions can lead to a birth injury like cerebral palsy or hypoxic ischemic encephalopathy (HIE).
Social determinants of health and chronic illnesses are even more prevalent in regions that are already marked as maternity deserts, which, in turn, place an added burden on expectant mothers who have limited access to healthcare options.
The Underlying Causes of Maternity Deserts
The states registering the highest incidence of maternity care deserts include North Dakota, South Dakota, Alaska, Oklahoma, and Nebraska. These states predominantly feature rural populations, as revealed in the March of Dimes report.
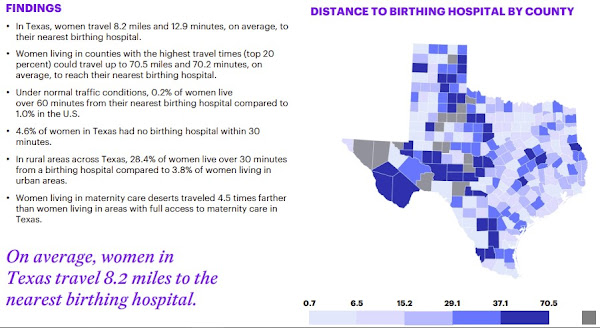
For instance, in North Dakota, a substantial 71.3% of rural residents are situated at least 30 minutes away from a maternity care hospital, with an average travel distance of 54.7 miles, Dr. Cherot stated. In terms of care quality, New Mexico displays the highest rate of substandard prenatal care, closely trailed by Hawaii, which is a state that’s expensive to live in.
It’s noteworthy that a socio-economic and racial dimension is also at play. Dr. Cherot pointed out that Black and Native American women experience the most unfavorable outcomes, coupled with the highest incidence of inadequate prenatal care.
Ignoring Prenatal Care Due to Restricted Choices
An expectant mother residing in a maternity desert is compelled to visit the nearest county where care is accessible. In a few cases, this might involve crossing just a nearby county boundary. For many others, this could entail hours of travel, a situation fraught with danger during active labor or a medical emergency. It is well-documented that a leading cause of HIE and cerebral palsy is a delay of delivery when the baby is suffering from fetal distress. Forcing an expectant mother to travel long distance to deliver her child only increases the risks of these serious birth injuries.
Expectant mothers in these maternity deserts often attend a fraction of prenatal appointments.
Some expectant mothers may consult community midwives who lack formal licensing and consistent training. Alternatively, they might head to the nearest emergency room whenever they sense something is amiss, without the benefit of continuous care from a regular provider.
Even more alarmingly, a number of women may bypass prenatal care altogether. Dr. Cherot remarked that expectant mothers who forego prenatal care face three times higher odds of experiencing adverse outcomes.
In some instances, women go into labor while en route to a hospital. Dr. Kristy Acosta, a Family Medicine/OB practitioner at the Brownfield Regional Medical Center in Texas, reported that it's not uncommon for her to receive a call that a mother has given birth at a gas station. She then awaits their arrival at the emergency room.
According to the article, Kali Bautista, a resident of Terry County, Texas, delivered her child while dwelling in a maternity desert within the state. Her hometown is situated 30 to 45 minutes away from Lubbock. She shared her concerns saying that one of her chief fears was what would happen if she went into labor during the journey.
Staffing Shortages and Obstetrician Burnouts
The closure of hospitals or maternity units can be attributed to a variety of factors, predominantly revolving around a shortage of trained staff. According to March of Dimes' press release, obstetricians exhibit one of the highest burnout rates within the healthcare industry, complicating the process of attracting and retaining staff.
In just one year, the count of birthing hospitals has dwindled by 4%. Since 2018, as many as 301 birthing units have ceased operations. Experts indicate a serious shortage of qualified OB-GYNs across the United States. Moreover, as a significant proportion of doctors are nearing their retirement age, a wave of retirements is imminent in the upcoming years. And there is a clear decline in the number of new OB-GYNs entering the workforce to fill the void.
While midwives offer valuable support in the birthing process, they do not engage in surgical procedures like operative vaginal deliveries, cesarean sections, cervical cerclage (suturing the incompetent cervix to prevent premature birth), handling the birth of a breech baby, or other complicated aspects of obstetric care.
Escalating Costs of Care and Inadequate Financial Reimbursement
Increasing costs of prenatal care and insufficient reimbursement also contribute to this problem, as shown by the March of Dimes report. Only about half of the births in maternity care deserts are covered by Medicaid, as per the American Hospital Association's data. This implies that hospitals receive lower reimbursement rates, leading to financial losses when offering obstetric care.
Dr. Cherot stated that the issue ultimately boils down to economics. Purely for economic reasons, the healthcare system in the country is failing to accord the necessary priority to the well-being of mothers and babies. Maternal health is a concern that reverberates throughout the society, and the March of Dimes report underscores that each one of us has a role to play in safeguarding the health of both expectant mothers and babies.
Miller Weisbrod Olesky has a long history of helping victims of cerebral palsy and HIE
Whether the birth injury is caused by a lack of proper prenatal care, a delay due to the lack of proper transfer from a ill-equipped hospital or the mistakes of the medical team during labor and delivery or shortly after childbirth, our experienced cerebral palsy and HIE birth injury attorneys have helped families all across the United States that are struggling with the reality and costs of raising a disabled child.
Families have the right to know if their child’s cerebral palsy or HIE were caused by mistakes of doctors, nurses and hospitals. For absolutely no initial cost to you and your family, we will conduct a detailed review of the medical records and all other available information to determine if your child’s birth injury was avoidable. There were never be a fee unless and unti we receive a successful money settlement for your child.